Medically Assisted Reproduction
- /
- Medically Assisted Reproduction

Assisted Reproduction Technology
In the normal physiology of a woman, during a regular cycle, one egg matures each month. The goal of in vitro fertilization (IVF) is to obtain as many eggs as possible, aiming to increase the chances of treatment success. To achieve this, medication is used to stimulate the ovaries. It is important to emphasize that the stimulated eggs would have grown and died that month anyway, so ovarian stimulation does not reduce the ovarian reserve for the future.
PHASE I: OVARY STIMULATION
During the stimulation phase, daily injectable hormonal medications will be used for about 8-14 days to stimulate the ovaries to produce as many mature eggs as possible. The goal is to create a greater number of high-quality embryos, thereby increasing the chances of pregnancy.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are both naturally produced in a woman’s body, but in these cases, with the help of medication, doses higher than physiological levels are administered to obtain more eggs. During this period, the doctor will monitor the growth of ovarian follicles through ultrasound examinations and estradiol level measurements to adjust the medication doses accordingly. To complete the ovulatory maturation process, you will also receive a dose of either human chorionic gonadotropin (hCG) or Lupron, depending on your individual protocol. This is important because the egg retrieval will be scheduled based on the expected time of ovulation, which is calculated to occur approximately 34-36 hours after administering this injection.
PHASE II: EGG RETRIEVAL
The doctors will perform this procedure in the facilities of our clinic. On the morning of the egg retrieval, you will meet with the doctor to review your protocol. You will also meet with the anesthesiologist, who will review your medical history and accordingly administer the appropriate type of anesthesia during the procedure.
Egg retrieval is a procedure that lasts about 15-30 minutes, during which the doctors use a needle to aspirate the follicular fluid, which contains the eggs. The aspiration procedure is performed under ultrasound guidance. You will wake up after 15-30 minutes, able to walk on your own, but it is important that someone accompanies you home, as you will have been under anesthesia and cannot drive yourself.
Sperm collection: The andrology laboratory staff will receive the fresh sperm sample, or in cases where you are using previously frozen or donated sperm, all details will be verified with you. Then, sperm preparation for fertilization of the eggs will be performed.
PHASE III: FERTILIZATION
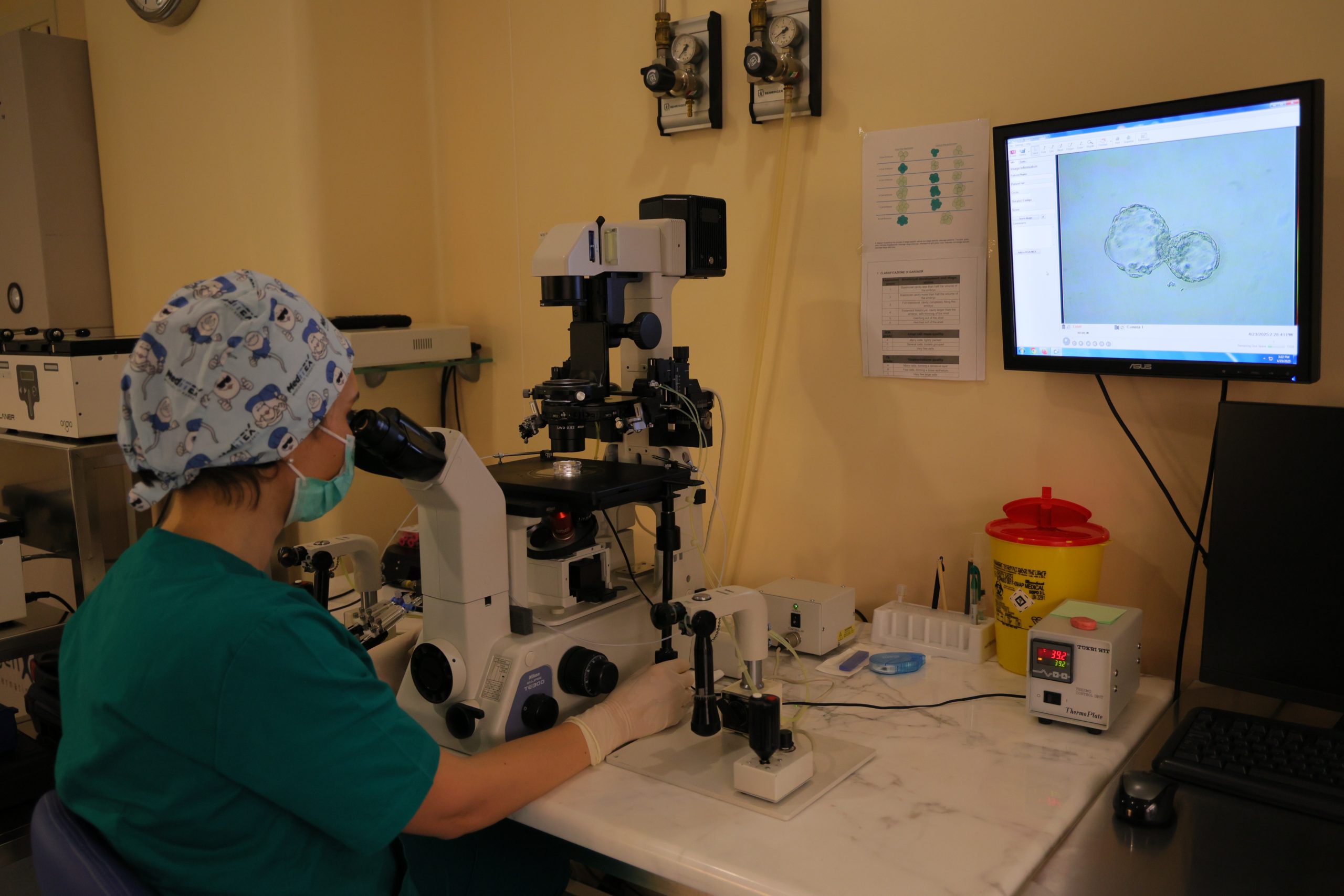
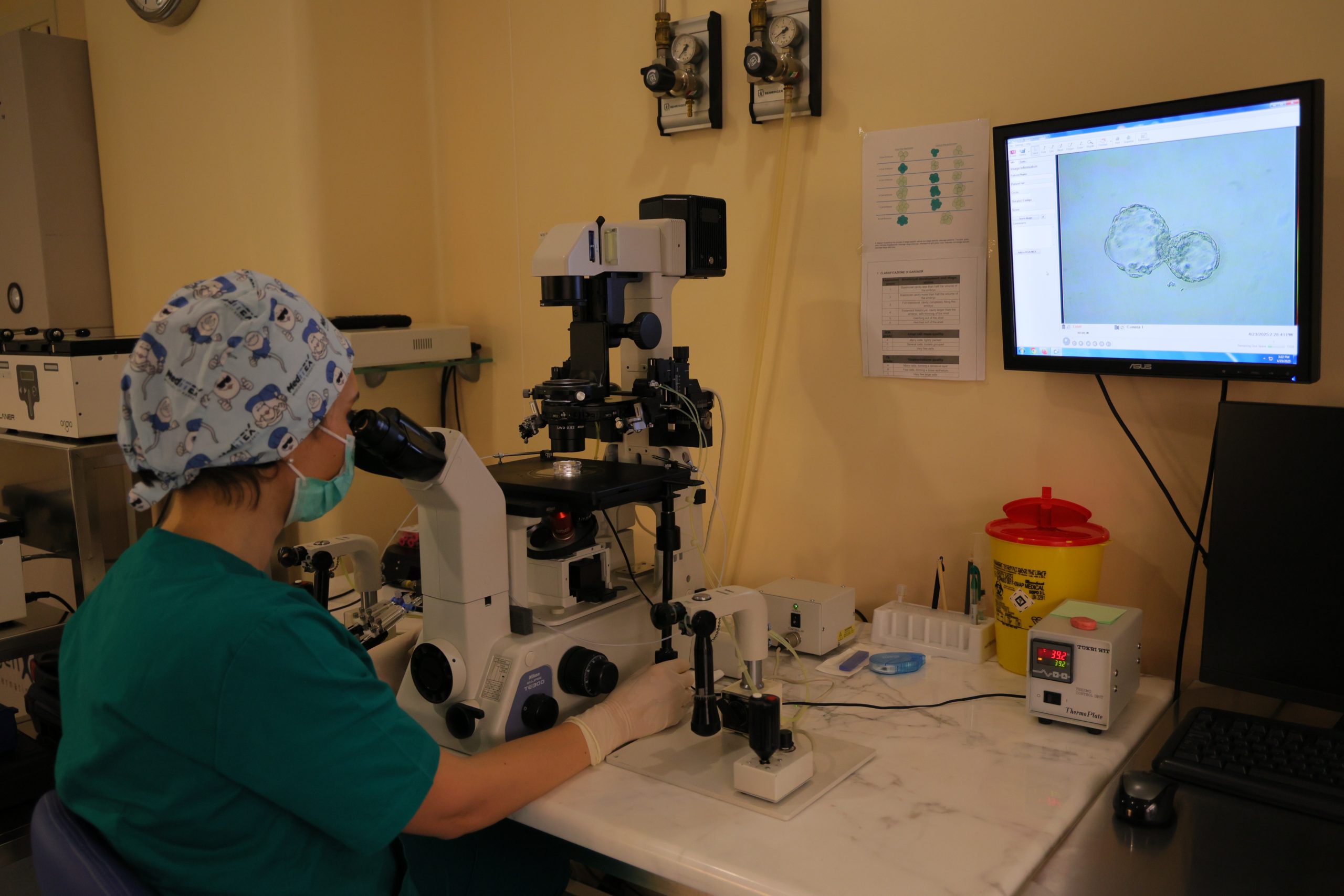
The embryologists will select and prepare the eggs and sperm. There are two techniques that can be chosen for fertilization: conventional insemination or intracytoplasmic sperm injection (ICSI). The doctors will discuss with you which technique will be used depending on the quality of the sperm.
Conventional insemination: In this case, the embryologist places the eggs and sperm together in a Petri dish, allowing the sperm and egg to find each other and fertilize naturally.
Intracytoplasmic sperm injection (ICSI): This is a process in which the embryologist injects a single sperm directly into the cytoplasm of each egg, and fertilization is monitored in the following days.
PHASE IV: EMBRYO DEVELOPMENT
Embryo development begins after fertilization. The embryologist examines each embryo, monitoring them for 3 to 5 or 6 days. The progressive development is then closely followed: on day 2, the embryo is expected to have two to four cells; by day 3, it should have six to eight cells. After the eight-cell stage, rapid cell division occurs, and the embryo reaches what is known as the blastocyst stage on day 5 or 6.
The goal of the embryologists and doctors is to transfer the highest-quality embryos to give you the best possible chance of success.


PHASE V: PRE-IMPLANTATION GENETIC ANALYSIS PGT – PRE-IMPLANTATION GENETIC TESTING (DETECTS CHROMOSOME ANEUPLOYIDES)
Embryos created in the laboratory through in vitro fertilization can undergo preimplantation genetic testing (PGT). This genetic analysis involves detecting aneuploidies (numerical abnormalities) across all 24 chromosomes of the embryonic cells. A small number of cells are biopsied from each embryo on day 5 of development and sent to a genetics laboratory for analysis. The ultimate goal is to transfer only healthy embryos into the uterus.
This process helps to reduce the risk of:
IVF treatment failure.
Recurrent miscarriages.
Birth of children with Down syndrome or other aneuploidy-related syndromes.
PGT is primarily recommended in cases where:
The woman is over 35 years old.
A woman has undergone several unsuccessful IVF treatments.
The woman has experienced recurrent miscarriages.
PGD – Preimplantation Genetic Diagnosis (Detects genetic disorders for a specific single gene)
PGD is a procedure that allows the identification of genetic abnormalities in embryos created through in vitro fertilization, before transferring them to the woman’s uterus. PGD is performed when the prospective parents are carriers or affected by a known genetic disorder, such as Cystic Fibrosis, Thalassemia, or others. In this case, the embryo is specifically tested for a particular genetic defect in the affected gene, ensuring that only healthy, unaffected embryos are transferred into the uterus.
The procedure is performed in the same way as for PGT. The embryos from which the cells are biopsied are preserved by deep freezing in liquid nitrogen until the genetic laboratory results are available. Only healthy embryos without genetic abnormalities are then transferred into the woman’s uterus.
PHASE VI: EMBRYO TRANSFER
Embryo transfer is a very simple procedure that takes only a few minutes to perform. The nurse will provide you with the necessary instructions on how to prepare, for example: your bladder needs to be full in order to obtain a clear ultrasound view of the uterine contours, which helps ensure optimal placement of the embryos.
Prior to the procedure, you will have agreed with your doctors on the number of embryos to be transferred. The embryos are loaded into a thin catheter in the embryology laboratory, which is adjacent to the transfer room, and are then carefully released into the uterus under ultrasound guidance.
After the embryos have been transferred, the embryologist performs a final check under the microscope to confirm that no embryos remain in the catheter. The nurse will then give you detailed instructions regarding your medications for the next two weeks, up until the pregnancy test is performed.
PHASE VII: PREGNANCY TEST (Β-HCG)
Two weeks after the embryo transfer, you will take a pregnancy test. This test is performed by taking a sample of peripheral blood and measuring the level of β-hCG, which confirms or rules out a pregnancy.


